I love medicine; it’s doctors that drive me crazy
December 1, 2009 at 2:41 pm | Posted in Uncategorized | 4 CommentsThe nicest thing about family is that you can tell them exactly what you think about everybody else in your life, without concern for how your opinion would reflect back on you if your colleagues somehow found out. From which you can safely infer that there’s a whole lot more going on in my head than I feel comfortable talking about either here or at work.
I never forget that I’m not truly anonymous here, even if the vast majority of my readers have never met me, and have little to do with neurosurgery. All you have to do is look at the page view statistics to know that the minute I say something the least bit gossipy or potentially scandalous, word somehow gets out and suddenly I have 10 times the usual number of visitors. So I’m extraordinarily careful these days.
It’s probably commentary enough, that I feel it necessary to tread so carefully.
In any event, it was nice to get all of it out of my head, finally. Some days I just really hate the culture of medicine, and particularly medical training.
On a related note, I’m appalled at the lack of thought that my mom’s primary care doctor has given to the prescriptions she writes for my mom. My mom is on a fixed income, and is currently in the Medicare “doughnut hole” of prescription coverage.
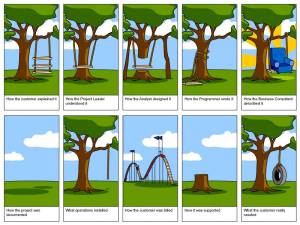
(For the uninitiated, this means she has exhausted her basic prescription coverage, and now has to pay 100% of the cost of her prescriptions until she reaches some expenditure cutoff, and then Medicare will pay again. Medicare Part D is possibly the most idiotically designed public policy I’ve seen in my lifetime. In fact, I’m reminded of this classic cartoon (click to zoom):
Although I anticipate that health care reform will be worse–my only question, in deciding whether to support it or not, will be whether it’s worse than what we currently have, and I think that would be difficult to accomplish. I guess that depends on how you define “worse,” though. In my view, worse means more physician paperwork for less actual care provided and fewer people covered.)
Anyway, back to my point. All of my mom’s prescriptions are for medications with no generic available, with the exception of one (which happens to be the single agent in its class). To make matters worse, one of them is a total scam product, where the pharmaceutical company took their prodrug that was coming off patent, lopped off an inactive functional group, and is now selling the metabolite as a whole “new and better” agent for the exact same indication.
Now that, just by itself, is enough to make my head explode. Seriously, any PCP who would prescribe that to a retired person living solely on Social Security should have to buy it themselves every month for every patient they prescribe it to, and pay the cash price. Then watch how quickly they learn not to be pawns of Big Pharma.
Then the other major medication she’s on is one of a class of second-line agents (for which there are no generics yet) for patients who don’t tolerate therapy with the first line class of drugs–all of which are available as generics. And you can guess the rest of the story…she’s never been tried on the first-line agents.
AAAARRRGGGHHHHH!
Not to mention that her PCP is a D.O., who as a group pride themselves on their primary care training and holistic approach to patients. So I figured she’d be in excellent hands.
And then I find out that she’s paying $500 a month for her prescriptions. And in fact is trying to skip days here and there so that she can get to January (when she’s covered again) before she needs refills in order to pay for some much-needed maintenance on her house.
And her daughter is a doctor. Of medicine AND pharmacy.
If even she can’t get anything besides cookie-cutter, Pharma-driven primary care, I can only imagine the kind of reckless prescribing other people’s parents are dealing with.
Seriously, some days I wish primary care could be pickier about who it trains.
Intuition + knowledge
November 24, 2009 at 12:02 am | Posted in Uncategorized | Leave a commentMy most recent call night was one of the easiest I’ve had since I started here. Not because nothing happened (it was actually quite eventful), but because I knew what to do about everything that did happen. Also because the calls I got involved, for the most part, real problems. Our floor nurses are notorious for hammering us with pages about clinically unimportant issues, simply because they feel neglected. So “crying wolf” is always on the differential. But for whatever reason, this last call night I somehow just knew the problems were real.
Parenthetically, this is why I like EMRs when dealing with floor patients. Nothing surprises the floor nurses like YOU calling THEM about an issue before they get a chance to page you. Not that I’m able to do that often, as the ICU and ER patients generally take up all my time. But it’s fun when I can.
Anyway, that night was a steady stream of badness, all across the hospital. First, we got a subarachnoid hemorrhage that actually turned out to be aneurysmal. It’s always more satisfying to find an aneurysm, because at least then there’s something we can do about it, besides just sit around twiddling our thumbs with medical treatments, waiting for the patient either to get better or go into vasospasm. I also like spontaneous subarachnoids because they’re an automatic two-fer, procedurally, since they all get an arterial line and a central line.
The poor lady’s husband was beside himself with worry, though. I nearly cried, myself, while I was getting consent to clip it. Mostly because I had to bring up all the complications that could happen, and was unable to reassure him beyond saying that her surgeon was excellent and that we would do everything in our power to ensure the best possible recovery for her.
And then another patient who was scheduled to be discharged to rehab the very next day developed a massive hemorrhage, and lost all brainstem reflexes within an hour. She had been talking on the phone to her husband just a couple hours prior, and then she was comatose when the nurse came in for her next neuro check. Another difficult family conversation.
Then another patient had a urethral injury due to inadvertent traction on his Foley catheter at some unknown recent point, with about 2 liters of hemorrhage into his bladder. It presented in a benign manner, with somewhat decreased urine output, but not below the 30mL/h threshold that triggers clinical alarms. But it had become bloody as well, for no apparent reason. So I asked the nurse to flush the tube, and she reported back that she was only able to get a small amount of output after doing so, and that it was full of clots. She then scanned the bladder and found >500mL of volume still inside, and noted that he was bleeding around the Foley. So I came over to examine him, and found that his abdomen was also very firm and distended (I know, a neurosurgeon actually examining an abdomen…surely a sign of the coming apocalypse). It was definitely time to call urology. So I did, and the urology resident came over, made sure the bladder wasn’t ruptured, took out the Foley, placed a Coude, and irrigated the bladder until all the blood came out. Thank God that nurse caught it when she did.
And then two peds patients with head injuries. One, the teenager, was not seriously injured but was dramatizing the concussive symptoms a bit. (When you deal with the whole spectrum of deceit, from simple disingenuousness to outright lying, as you do in retail pharmacy, the BS sensor gets very acute.) I decided to let it go, as we would be watching him overnight regardless of his mental status.
The other pediatric patient was seriously injured. It was unclear at the time I left how serious the injuries were, but to me they did not seem serious enough to require surgery, or to result in diffuse axonal injury. But anytime there’s a child involved, people get excessively worked up over it, and I’ll admit the mechanism of injury was quite dramatic.
On a more mundane note, we are all still adjusting to writing our notes electronically. Some are adapting more quickly than others. Despite the system being the same as at UW, this place hasn’t developed any note templates to automate things at all. So we each have to make our own templates, and every day we have to manually import the latest vitals, meds and labs. IMHO, this is a direct result of having an IM person in charge of implementation. Those medicine people have a much lower patient-to-resident ratio than we do, and they have much more time to write their notes, as well. Our usual MO is to write notes and round as quickly as possible, so we can get to the OR/clinic/bedside procedures/whatever as quickly as possible. The extra time required to write notes and import data by hand doesn’t affect their ability to function effectively nearly as much as it does ours.
Meanwhile the VA remains as slow as ever. I feel a bit guilty being over there, knowing how short-handed it leaves the university hospital. But I’m getting a lot of studying done, and my current goal is to be able to distinguish reliably between a radiculopathy and a peripheral nerve issue based solely on the clinical exam. I have a general grasp of it already, but I want to be able to simply look at a bunch of exam findings, and remember them as a unit–the diagnosis they represent–rather than as individual pieces. Which requires spending some quality time back down in the weeds of 1st and 2nd year, and integrating all of that with the hundreds of patients I’ve seen and will see in clinic with undifferentiated back pain, weakness or numbness.
I’m not a fan of the spine aspect of neurosurgery. But if I have to learn it, I’m going to learn it like the back of my hand.
Shhhhh! It’s a secret.
November 20, 2009 at 5:27 pm | Posted in Uncategorized | 1 CommentWhen I first moved here, I thought this place was going to be like the poor white trash cousin of its neighboring state, with which I’m fairly familiar.
But it turns out I’m wrong. In fact, it’s a mystery to me why millions of people chose to live there instead of here. This place is much prettier, and has a far more tolerable climate. Not to mention better skiing within a reasonable driving distance. As a city, it’s missing only a Chipotle. Everything else is here.
Now, granted, the lack of a Chipotle (or its copycat, Qdoba) is a big void. But I lived for two and some-odd years in New Orleans without one. And I’m confident one will find its way here eventually (unlike NOLA with its distaste for non-local franchises, Starbucks in particular).
The city isn’t at its best this particular time of year. But the department showed itself off well at its last interview day. I was trying to view the day from the perspective of an applicant, and I have to admit, the morning conference was impressive. And the ICU here is as nice as anything you’d find elsewhere. Really, all it would take is one competitive applicant to be impressed and vocal about it, to put this place on the map.
For lack of a nail…
November 2, 2009 at 11:30 am | Posted in Uncategorized | Leave a commentWell, one minor mystery solved. I have this old Perkins loan from med school for which I never got one single bill or notice of delinquency from Tulane. The first notice I ever got for this particular loan (and if you have as many as I do, it’s hard to keep track of them all. In fact, I had made a point of keeping them all with one lender for that very reason. But a Perkins loan is directly from the government, not through a third party lender, so I didn’t have that option. And I’ll be honest, I completely forgot about it.) was from a collection agency who wanted to tack on an additional $10,000 to the amount owed. This represents over a 50% fee on the original balance. So I told Tulane I was willing to repay the loan to the school, along with any interest that had accrued, but no way in hell was I paying this usurious collection agency a single penny.
The school said it had sent bills, and I believe them. But what had happened to them all? Certainly I was getting all the med school’s requests to donate money.
Well, it turns out that the Financial Aid office for the main campus (not the med school) was sending the bills to Mystreet NW instead of Mystreet NE in Seattle. And of course Seattle’s crappy postal service never figured it out, even though it surely is a very common error in a city where streets are named by quadrants.
And unlike the postal service here, which has managed to forward all of my mom’s packages to me, even though she addresses it to someplace 50 blocks away.
snow day
October 31, 2009 at 10:14 am | Posted in Uncategorized | Leave a commentI was going to write this Thursday, but held off for reasons that don’t matter so much today. Plus this past week contained the previously mentioned Bring Your Ativan to Work Day. So it’s been altogether a very painful 5 days.
Nonetheless, I’ve decided that I really like Fellowship City. I came to this conclusion Thursday afternoon as I was at lunch, staring at the snowglobe-esque scene outside the hospital. I love snow.
I mean, I do like not having snow for a lot of the year. But my family likes to live in places where it never snows, and this is yet another way in which I’m the black sheep. So I was all excited about the mini-blizzard Thursday afternoon. Particularly since it looked pretty and then melted before creating any rush-hour commuting drama.
Although the neurologists did cancel their grand rounds the following morning because of “inclement weather” (which by that time was sunny and well above freezing again.) Wimps.
Also, I have a garage here, so there’s none of that annoying car window-scraping to be done when it gets below freezing. Which makes all the difference. And the place where I go to swim in the morning (when I go) manages to keep the area around its semi-indoor pool warm enough to make walking from the building to the pool a realistic endeavor, even when it’s freezing outside.
So it’s an easy place to live, with respect to what I look for in a city.
I know there hasn’t been much talk on this blog lately about anything important. But that’s because the drama around here right now is not about me. And I don’t care to become an object of gossip, even if everyone does need something else to focus on.
NOLA 2009
October 25, 2009 at 1:49 am | Posted in Uncategorized | Leave a commentOK, my neurosurgery peeps. I know you want to know where to go in New Orleans.
Because you don’t want to go to Bourbon street. Really. It’s full of tourists and it smells like vomit. So here are some suggestions, courtesy of me (and people who are much cooler than me).
Food:
- Port of Call
- Franky and Johnny’s
- La Crepe Nanou
- Commander’s Palace (of course)
- Brigtsen’s
- Cafe Degas
Drinking/Hanging out:
- Balcony Bar
- Monkey Hill
- Bulldog
- Superior Grill
- Dos Jefes Cigar Bar
- F&M’s
Dancing/Music:
- Tipitina’s
- Maple Leaf
- d.b.a.
- Twi Ro PA
Coffeehouses:
- CC’s on Magazine/Jefferson (my favorite place to study)
- Rue de la Course
- PJ’s
- Cafe du Monde (have the beignets, or don’t bother going)
There are more. You pretty much can’t go wrong anyplace on Magazine or Tchoupitoulas (“chop” in local parlance).
And last I heard, Joe’s next to Tulane Hospital no longer exists (sniff). Good old Lab J. There’s some new hangout a couple streets over, now. Handsome Willy’s, I think it’s called, but I remember it being more of an LSU med hangout than a Tulane one. And I doubt it has an x-ray viewbox like Joe’s did.
Anyway, have fun, and laissez les bon temps roulez!
Taking work home
October 24, 2009 at 11:45 pm | Posted in Uncategorized | Leave a commentWe had one of those deaths earlier this week that haunt you. The kind where you keep going over everything that happened, wondering what it was that you missed, and whether there was something you could have done differently to change the outcome. Because this was a patient who did not seem sick enough to die.
Hopefully we’ll get some answers from the autopsy.
And the fact that I see so much death that I can categorize it into “disturbing” and “non-disturbing” kinds, is itself a little disturbing.
On the distal side of the line
October 19, 2009 at 10:47 pm | Posted in Uncategorized | 3 CommentsIt’s a rum and coke night tonight. Except I’ve already drank as much as my puny tolerance will allow on a worknight. Which was about a quarter of a shot.
I have this bottle of dark rum that I bought in Nicaragua (6 and a half years ago), and it’s hardly been touched. In fact, it sat on my kitchen counter entirely untouched for 5 years. And then came the Scramble last year. After which it seemed a fitting time to break it open and have a glass. I figure when people tell me to go have a drink, I’ve probably crossed over from the simply crappy to the truly craptastic, and a little lidocaine for the psyche is in order.
Today was one of those kinds of days. Although now I’m just drinking plain diet coke again.
I’m not sure where to start with today’s events. But I’m going to be a little more frank than usual. I blame the alcohol. It’s possible that I drank the alcohol in order to blame it, but nonetheless that’s my story and I’m sticking to it.
First of all, there were plenty of people around, but no one to whom I could actually delegate any real work. We had an ER resident, who’s not allowed to consent anyone and can’t do any of the procedures that needed doing today. We also had a new foreign medical grad, who also couldn’t do any of the things that needed to be done, couldn’t even write orders because she wasn’t in the system yet, and in addition to that kept asking me if there was anything she could do to help. Which is twice as annoying when the person asking obviously can’t. We had one extra resident today, who showed up to run the list in the morning and then disappeared without doing any work. This particular resident is a master at avoiding work and evading responsibility for it. Although no one actually trusts anything this resident says, anyway.
I think that’s what bothers me most about this program. The residents are not a team. With a few notable exceptions, everyone is out for him- or herself. No one has your back, not even the chief. You would think that such difficult-to-please attendings as we have here would inspire a sense of camaraderie amongst the residents. But it seems to do the opposite.
But getting back to today. At about 1:30 I was trying to get some hemostasis on our new patient’s scalp wound when I got a spray of lidocaine, epinephrine and arterial blood right into my eye. Body fluid exposures are frankly a pain in the ass, and I had too much to do to deal with one today.
But I’ve worked in health care nearly all of my life, and the two things that have been pounded into my head year after year are handwashing and the importance of reporting all accidents, mistakes and occupational exposures. Plus, who can really be sure that this patient doesn’t have HIV or hepatitis? And it didn’t help that my eye actually hurt and I was developing a splitting headache.
And of course, just as I’m getting ready to head over to the Occupational Health clinic, I get a consult for an operative subdural in the ER. Damn it. I’m sitting there thinking, do I operate today, or do I get post-exposure prophylaxis and ensure that I can operate 10 years from now? I wouldn’t be able to do both. So I saw the consult, got the patient on their way to the OR, and headed over to Occupational Health. No sooner was I back than one of the attendings sent some random person over to observe me do a neurological exam on a patient. Then it was 4:30 and the chief wanted to run the list with everyone. This took an hour, between rounding everyone up, updating the list, and then actually going through the patients. No one was even consented yet for any of the procedures that needed to be done. So I was in the middle of doing that when I got a call from one of the attendings asking me why the procedure hadn’t been done on their patient yet.
Well, not really asking. More like demanding to know what I’d been doing, and telling me that what I had done instead was unacceptable. Which, message-carrying ethos or not, is an indefensible statement coming from anyone in a position of authority in a hospital. But it would have been counterproductive to point that out. So I just quit talking, and instead listened quietly until the subject moved on to what ought to be done now to solve the problem.
The only good way I’ve found to deal with other people’s anger is just to let it flow around and past you like an ill wind. It’s like walking out the door in Phoenix in the middle of summer. All of a sudden there’s a burst of hot, dry, hellish air, and you just tolerate it for a little while until you get someplace air-conditioned again. In fact, that’s exactly what I imagine in my mind’s eye as it happens.
Anyway, I ended up staying about three hours beyond signout in order to avoid dumping most of the work onto the on-call resident.
You know, the other thing this program needs is a more structured way of bringing people along from the knowledge level of a med student to that of a PGY-3. They really haven’t had to do that with the vast majority of their residents, but it’s the kind of thing that programs who routinely match AMGs straight out of school obviously have to do, and seem to do well enough.
Then again, they use a lot of AANS materials here that I don’t have access to because I’m not officially a resident. So maybe that’s where the teaching is.
Perspective
October 8, 2009 at 7:34 pm | Posted in Uncategorized | Leave a commentMan, I thought some of the criticism I’m getting is harsh. –Not undeserved, let me make that clear. Just very direct and with the bar always higher than wherever I am. But I’ve never been told by anyone that I’m not cut out for neurosurgery. Lacking in knowledge and skills, yes. But not fundamentally unsuited for the field.
Well, apparently, people do get told that.
Shunt this, all you naysayers
October 5, 2009 at 8:24 pm | Posted in Uncategorized | 2 CommentsYesterday I put in my first solo EVD. I know, I know, it’s freaking October, and this is my first? WTF?
My sentiments exactly. Continue Reading Shunt this, all you naysayers…
Partly cloudy and cool, with a 70% chance of social retardation
September 18, 2009 at 12:23 am | Posted in Uncategorized | Leave a commentYesterday, or maybe a couple of days ago–it all runs together when you take call three times in one seven day stretch, I had a rather long conversation with someone at work. Professionally, I like this guy, and personally we get along well. He’s also a very un-private person who talks freely about his life outside of work, so I know a lot more about him than he knows about me.
Well, the other day we were stuck together waiting for a patient to get scanned, and he started asking me all kinds of questions about myself. What I think of this program, whether I want to stay here, where I came from, why I’m interested in neurosurgery, do I have kids or a significant other, etc. Those of you who know me, know that when I talk to people, I tend to reflect their tone and level of openness in my own speech. So I pretty much told him exactly what I was thinking, which was not particularly wise or advantageous of me, politically. And socially it was entirely retarded of me, although at the time honesty seemed like the only respectable option.
But oh well, I guess at some point you have to let down your guard with people. Particularly when your job consumes as much of your life as neurosurgery does.
No man is an island, not even if he’s a Republican
September 17, 2009 at 10:32 pm | Posted in Uncategorized | Leave a commentGo Margaret and Helen! I just love those two old ladies and their liberal rants. Then again, I just like old people in general. They crack me up, because they say whatever the hell they want and really don’t give a shit whether you approve or not. Which means that often times they say exactly what I’m thinking.
Except for my own parents, who drive me nuts with the exact same behavior. The difference is that I feel like their behavior reflects on me somehow. I worry that people think I’m secretly harboring the same opinions, because, you know, that’s the talk I heard at home. And the reality is that my own values contrast pretty starkly with theirs in many ways.
Of course, the further away they get from the economically sheltered life of talented, intelligent and well-educated middle age adults, the less Republican their views become. In contrast, there’s no explanation for my own political views, given that I’ve always led a fairly sheltered life in this respect. I’ve just always been more aware of how easily it can all slip away in one random piece of bad luck, one random act of God, one natural disaster where you happened to be in the wrong place at the wrong time.
Certainly, there’s an element of individual control in all of these situations. You can do like I did in New Orleans, and be aware what the risks are and pick a place to live that minimizes your risk of loss or harm. But even so, your risk is significantly affected by other people choices as well, which you can’t control. I didn’t have control of levee maintenance, or the city pumps. I didn’t choose to try and piggyback Tulane’s entire medical curriculum on top of some other school’s very different educational philosophy and infrastructure. I didn’t choose to bring the entire school back before there was a sufficient clinical volume and infrastructure to provide adequate clinical exposure and teaching.
But these are the kinds of decisions where the right choice is only evident in retrospect. And what’s done is done. My point is that I’m acutely aware of the randomness inherent in life, and the whole point of having a safety net is that you never know when you’re going to need it. And chances are that no matter how invincible and in control of your life you feel now, at some point you will fall.
This was brought home very starkly this past week, in which a resident in one of our programs sustained a severe brain injury. He had done everything right, and still ended up in our ER with the kind of head injury that could have been fatal, or worse, nonfatal but neurologically devastating. I had seen a similar thing happen at UW, although with a more severe injury and a different outcome. That’s one of the hardest parts of neurosurgery: the knowledge that no matter what you do or don’t do, only occasionally are your patients totally normal again.
But that’s not the hardest part. The hardest part is knowing that you made them worse off than they would have been without your intervention. I mean, it sucks that we have basically the same number of patients as the general surgeons with only 1 resident in house compared to their 4, so it always feels like you’re being pulled in 5 directions at once. And it sucks to have to explain in the morning why all 5 of those things didn’t get taken care of all at once like they needed to be. But when you’re home and rested, it’s the people you harmed that haunt you.
Not that I have a lot of experience with that as yet. Mostly it’s vicarious, when I examine somebody that has a new deficit that wasn’t there prior to the surgery. But the attendings mentally flagellate themselves whenever it happens, and you can see it in their eyes. Often times, they’ve done absolutely nothing wrong, and this is just that 1 in however many cases in which this adverse event occurs. But for that one patient, it doesn’t matter how low the odds were. Nor is it their fault, yet they have to live with the consequences.
So how you can be a Republican, and against truly universal health coverage, as well as other social safety nets, when every day you see before you evidence that we’re all just a heartbeat away from the kind of loss that lands you on welfare or disability for the rest of your life, is a mystery to me.
Patient management
September 8, 2009 at 10:33 pm | Posted in Uncategorized | Leave a commentToday was a bad day, for reasons that will probably seem a little ridiculous/arrogant/spoiled/some combination thereof. I’m pissed off with myself today because two of my patients were worse off this morning than they were yesterday.
This kind of thing does not happen to me. My patients who should get better, do. And those who get worse or die do so because either we can’t save them no matter what we do, or we’ve chosen patient comfort as the treatment goal, rather than palliation or cure.
It’s those damn lungs again. When patients start having pulmonary issues, some part of my brain goes, “Ack! Physics!” and just shuts down. Which is silly, because I have a decent intuitive grasp of the processes involved, and am certainly capable of figuring out what’s going on. I just, for whatever reason, feel intimidated by pulmonary issues, and therefore have a tendency to stand back and let other people solve that particular part of the patient’s critical care management. And the end result is that I’m not very good at sorting out ICU patients once their lungs start causing problems.
This must stop.
As an intern, I was one of the ones whose patients rarely did poorly, and I like to think that it was because I was on top of their care. I knew how to keep a small problem from becoming a big one, and could tell when something looked bad but didn’t mean anything. And also, equally important, when something that seemed small and insignificant was actually an early warning sign of decompensation somewhere.
I do not have that level of clinical insight yet with critical care patients. So I don’t know when to push back on a plan that I’m not sure is correct. I don’t know at what point to call and say: the plan is not working, we need to reassess. Nor is it even clear to me sometimes exactly what part of the plan is not working and needs reassessment.
Part of the problem is that some attendings’ plans seem to work better and more consistently than others. And I can’t quite put my finger on why that is. All I know is that with some attendings, patients always get better, the plan is clear and either I understand what’s going on and how to deal with it, or there is clearly a new problem. With other attendings I end rounds more confused and fragmented in my thinking than when I began.
But really, that’s no different than when I was an intern dealing with various chief residents. However, toward the end of intern year, I knew what I was doing, and so I relied far less on my chiefs for direction. Plus I knew how to manage the people above me in order to avoid getting a poor plan for the problem in question. (Anyone who says that you don’t manage your chiefs and attendings is either clueless or lying.) I’m gradually learning to do that here, but it’s one of a great many things I’m trying to learn at once. And it’s not an excuse.
So I’ll just have to keep reading and trying to understand, and make a more dedicated effort to master pulmonary critical care.
How long before I begin, before it starts, before I get in?
September 5, 2009 at 2:09 pm | Posted in Uncategorized | Leave a commentThis has been the strangest couple of weeks ever. First of all, last week I was assigned to clinic for nearly the entire week.
That’s why people go into surgery, you know. For the clinic. Continue Reading How long before I begin, before it starts, before I get in?…
Organizational psych 101
August 26, 2009 at 7:04 pm | Posted in Uncategorized | Leave a commentBack in college, my friends and I had a saying: it’s not what you do, it’s who you follow. Meaning that evaluations of how well you did your job are relative, and the key to looking like a star is to follow after someone who screwed up royally. And that if you have the bad luck to follow someone outstanding, it’s nearly impossible to look anything but mediocre.
The phenomenon isn’t obvious until you spend several years observing an organization with semesterly turnover of 30+ leadership positions, all of whom are people you know well and have worked with in numerous capacities. But once you have, it’s hard to miss. And frankly, I’ve never had an evaluation that wasn’t strongly influenced by where the person ahead of me set the bar. Not that that’s all there is to it, but it’s a far larger component than people seem to realize.
That’s all for today. I have reading to do.
Sticks and stones
August 20, 2009 at 10:53 pm | Posted in Uncategorized | Leave a commentNobody died last night. Nor did I grossly mismanage anyone. Yet conference was still a bloodbath.
Sleep deprivation is never fun, but for me the biggest toll of call is on my self-control. Post-call I’m much easier to push over the edge, emotionally. In fact, I routinely curse at all the cars around me over the slightest annoyance when I’m driving home the next day. I also take the opportunity to curse out anyone else who pissed me off during the preceding 30 hours. It’s cathartic. Plus it keeps me awake.
So it would have been pretty hard to deal with even the usual level of verbal aggression this morning. But today, for some reason, it was significantly worse than normal. I’ve been a lot of places now in my medical training, because of Katrina, away rotations and internship, and I actually haven’t seen anything quite like this since pharmacy school.
I’m also sensing some disturbing undercurrents among the residents and faculty. The other day in clinic I inadvertently walked into a conversation between a couple of attendings about alternative career options for one of the junior residents. At first I was alarmed that they were talking about me, because they changed the subject very quickly. But I’d heard enough that over the next couple of days it became apparent to me who they were talking about, based on the particular strengths of that resident. And obviously regardless of the resident’s identity, it was an inappropriate subject to discuss in front of another trainee. So it’s not like I can’t figure out what’s going on. I just don’t want to know.
My two cents
August 16, 2009 at 11:35 am | Posted in Uncategorized | Leave a commentI’m not an active part of this policy debate, but here’s my take on health care reform. Continue Reading My two cents…
Coming soon: bring your ativan to work day
August 15, 2009 at 5:49 am | Posted in Uncategorized | Leave a commentApparently I’m not TOO sleep-deprived at the moment, since I was up in time to go to work this morning, and I’m off today.
The hospital claims they will be fully implementing Cerner in a month or two. Everything all at once, including physician order entry. This should be interesting. Continue Reading Coming soon: bring your ativan to work day…
Fair vs right
August 9, 2009 at 7:13 pm | Posted in Uncategorized | Leave a commentI get a sense from the residents here that they’d consider it unfair if the place I just interviewed at offered me a spot. No one’s said anything overtly, but there’s the unspoken question hanging in the air, “why you? what makes you so special?”
And it certainly wouldn’t be fair. Then again, “fair” presumes that the playing field is level. But there’s nothing fair about whether or not we’re given an opportunity in life, there is only what we make of the opportunities we’re given, and what that says about us. And I know I’d make the most of that opportunity, and that it wouldn’t be wasted on me.
There’s a whole crapload of “unfair” I’ve been dealt in my life, and wouldn’t it be great if I really could build that metaphorical skyscraper of a career that I talked about so many years ago, despite it all.
WTF
August 8, 2009 at 1:03 pm | Posted in Uncategorized | Leave a commentYesterday one of the upper level residents said to me, in the middle of a conversation about all the things I’m doing wrong, “I know you’ve been sick this last week, but this is not Family Medicine. You can’t just go home or take a day off when you’re sick.”
I replied, “I’m aware of that, and I haven’t asked to. ”
Actually, the thought never even crossed my mind. I haven’t missed a single day, and in fact, I took q2 call during the worst of it.
So seriously, WTF?
Now, privately, I question the wisdom of coming in when I’m that ill, and caring for a bunch of patients who are already only hanging on by a thread. But I also recognize that it’s the best option available for my patients in the larger scheme of staffing availability, patient safety and so forth, and so I do it.
The way I see it, it’s not a matter of my image in the eyes of my superiors, or of my education. In fact, it’s not about me at all. It’s a matter of patient risk vs patient benefit of a team member showing up with a communicable illness. When you’re a student, the balance tips toward patient risk. You are less necessary even than the nurses, and your presence risks infecting the whole team, as well as any patients you care for.
But as a resident, patient benefit outweighs the risk; you are necessary and not easily replaceable if absent. And in a program where residents are already stretched pretty thin, there simply isn’t enough staff to cover. No matter how sick you are, you are better than the alternative.
However, this is not how most people see it. And since the decision of whether to come in or not is the same for me now as it would be for someone else in my current role, and for any future role I will have in medicine, there’s no point in trying to explain. People are remarkably unsophisticated when it comes to logical thinking, or ethics of any kind. But as they say, if you see an apparent contradiction, question your underlying assumptions first, because one of them is wrong.
Some thoughts
August 4, 2009 at 4:02 am | Posted in Uncategorized | Leave a commentAs you might expect, being a PGY-2 in all but name leaves very little time for blogging. Also there may be some really good news on the horizon (at least, I hope so!), and I’m just superstitious enough not to want to jinx it by talking about it. Irrational, I know, but there you have it.
My main impression so far is that neurosurgery here is harder than it needs to be. It’s true that at this place, you have to know your medicine and general surgery cold, as well as neurosurgery, and that’s certainly challenging. But they round for half the day here, which leaves very little time for actually getting any work done. I have mixed feelings on this subject, mostly because, while I recognize the need for oversight, it feels very haphazard and inefficient as a means of teaching about critical care, not to mention neurosurgery. I don’t feel like I’m learning much, other than that everyone has a different way of doing the same thing, and that good clinical judgment is a thing totally separate from being conversant with the literature of the field. There are many things done here that are no longer done elsewhere, and things done routinely elsewhere that earn me that “Are you f-ing crazy?” look here from staff and residents alike. And something tells me that being taught anything by someone in my position would be counterproductive as far as my intermediate-term goals are concerned. In other words, while my long-term goal is to become an excellent neurosurgeon, I can’t be excellent at it if no one will let me do it in the first place. Which requires a residency, and pissing people off is not the way to get one.
However, the pharmacists here are on top of their game, and would give their colleagues at Harborview a run for their money. They don’t round with us, but some of the protocols they have in place are well ahead of trends in the field, and they pretty much get what they want. But the pharmacy practice act in this state is clinically the strongest in the nation, so that’s not surprising.
July 30, 2009 at 1:48 am | Posted in Uncategorized | 2 Comments
Posting from my interview at Gigantic Hospital. I’m still mystified as to why they’ve invited me to interview. I must be their token outside applicant. I hope not, though, because this interview is costing me a fortune.
There is apparently no way to do this cheaply. My lone cost savings was on the plane ticket, for which I spent a large portion of the miles I had accumulated from last interview season in order to avoid paying actual cash. I was saving them for a rainy day, and well, it’s raining.
Anyway, this place is everything I’m looking for in a program. I just hope I’m what they’re looking for in an applicant.
Progress
July 26, 2009 at 12:49 pm | Posted in Uncategorized | Leave a commentAnother call night, another incremental gain in knowledge. This time I can tell that there’s a difference. Maybe no one else can, just yet. But I know that two weeks ago, this past night would have had me rending garments and comtemplating the consequences of skulking away at 3am and never coming back. (And before you pass judgment, we have a census that would support at least one additional resident every other year than the program currently is allowed. Plus we are the critical care service for the neuro ICU, including the neurology patients, in addition to handling neurosurgical issues. I like this, and I’m not complaining. But it is more work, and more stuff for me to learn.)
But somehow it wasn’t that bad. There were consults, there was power-paging by what seemed like the entire hospital while I was gowned and sterile for a line placement, and thus unable to answer. And during which I was also completely abandoned by the patient’s nurse for at least 20 minutes. Which is a fairly serious no-no of nursing, if I understand correctly. That nurse was obviously hating her life last night, as she was saddled with two brand new, unstable patients, both of which needed tubes and lines and labs and scans galore.
And yet, all of those things got done. Not quickly enough to make my senior happy with my work, but whatever. There are some situations where you’re just never going to win, and it’s important to know when you’re in one.
There were a few things that didn’t get done, but then again, it’s not like I slept at all, or even ate a decent meal. In fact, I’d been there 18 hours before I’d even had a chance to go to the bathroom. And I’d had to go since that morning.
I’m waiting for the day when we ask some patient to ” show me two fingers!” and the patient flips us off with both hands. It’s gonna happen someday, I just know it.
Anyway, I have one dictation left to do from today. And unfortunately, I’ve just discovered that the hospital’s dictation system doesn’t recognize the keypad touch tones from my iPhone. And I don’t have a landline, so I’m basically screwed until tomorrow morning. But hey, there’s only one this time.
And most importantly, no one died last night. In fact, nearly everyone is doing better this morning than they were yesterday. And nobody chewed me out for any of the changes I made overnight (although this is partly because I’m overcautious now.) But equally important, no one got mad at me for not making a change when one was needed, or not discussing it with someone senior to me.
I’m starting to think I might actually get the hang of this at some point.
My ego needs some fentanyl, stat
July 18, 2009 at 6:19 pm | Posted in Uncategorized | 1 CommentIt’s been a long couple of weeks. Longer because I stayed far later than normal a couple of times in order to learn some new things. Like invasive line placement, a skill at which my lack of experience was apparently quite unexpected. UW doesn’t give its interns much opportunity to place central lines or arterial lines. But as it turns out, it’s not actually that difficult.
I’m not keeping very close track of my overall hours, since it really doesn’t matter. But I think the schedule I’m on involves alternating 100- and 60-hour weeks. Which isn’t bad, compared to what my schedule might have been like elsewhere.
Right now, I’ve got several very irksome problems:
- It’s been over a year since I worked as a physician, and the mindset is completely different from that of a pharmacist. Granted, it’s a better fit than pharmacy, but there’s still an adjustment to be made. Another aspect of this is my habitual use of weasel words. I got in all kinds of trouble in pharmacy school for making definite statements in response to drug-related questions. And I remain persuaded that few things in medicine (or surgery) are truly black-and-white. But there’s no Heisenberg principle in surgery. Either it’s operative, or it isn’t. And either you operated, or you didn’t. There’s no shadow world where it may be either case in the future, or could be both at once. So the weasel words have to go.
- There’s also a huge difference between being a trainee and being a fully independent professional, legally responsible and expected to make my own decisions. I’ve spent the last year making my own decisions, answerable only to my own conscience and a court of law. It’s hard to regain the balance I had finally struck as an intern, between knowing when to simply do something I knew was correct, and knowing when to ask permission anyway. So right now I’m getting very mixed messages on how I’m supposed to behave: I don’t run things past my seniors enough AND I’m not independent enough.
- On top of this, there’s a lot of stuff I flat out still need to learn.
- There’s also a lot of stuff I know, but can’t recall with enough facility at the moment due to the stress of all these other things I’m trying to get right.
So, you know, the going is a bit tough right now. And there are some days when I understand why residents quit or transfer into other fields with such frequency. It’s hard to face seven years of feeling like an idiot about some thing or other every day. Much easier to break it up into smaller pieces, like a medicine residency and fellowship, where at least in the middle you get to feel like an almost-attending.
But I’m not going to be one of those people. For one, I have an abnormally well-developed tolerance for delayed gratification. And secondly, I can’t really picture myself doing anything else. At least, nothing else that doesn’t require a residency that would make me go postal (integrated vascular spots are too scarce to be a realistic option).
And don’t even talk to me about ENT. Blood, guts, vomit, stool, smushed brain: none of those bother me much. Earwax, however, nauseates me to the point where I have to put the scope down and leave the room. It makes no sense, but we all have our kryptonite, and that’s mine.
I’ve learned a lot already, in just three weeks. And now I have this weekend free to do some actual book-learning. Hopefully it’ll make the next two-week sprint a little less painful to my ego.
Ask the right question
July 10, 2009 at 12:36 am | Posted in Uncategorized | Leave a commentI survived my first call. There was one death on the service, an assault victim-turned-homicide for whom there was nothing we could have done. And one ICU transfer that I’m not entirely sure was inevitable. As far as I can tell, the rest of the patients were not worse off in the morning for the decisions I’d made overnight, although there were a couple of instances where I wasn’t able to defend myself adequately when put on the spot, though that doesn’t necessarily mean I was wrong. The number of consults was about what you’d see on a light night in Seattle, but the process is far less streamlined here, so it seemed like a lot more work. In fact, pretty much everything here seems take a lot more effort to get an acceptable result.
And then list is pretty long right now, which meant that there was a lot of work aside from the consults, and there were a couple of things that didn’t get done. Which is never a happy thing to have to report in the morning.
And now I need to come up with a research project. I was hoping that I’d be inspired by some case that came in while I was on call. But frankly, the question that kept popping up in my head was, how many days is one’s life shortened by each overnight call? Does it age you an extra week or so? Or does it just feel like it ages you excessively, without actually doing so?
By far, though, the biggest surprise was how much energy I still had the next day. I didn’t sleep, and yet physically I could have gone at least another full day. Mentally, probably not. But that has more to do with where I am on the learning curve with all this stuff than anything else. In time, there’ll be fewer things I have to think my way through from scratch, and I’ll become physically exhausted well before I run out of gas mentally.
As an aside, that’s why I think hour limitations aren’t such a bad thing overall for interns, and why I don’t think they work as well for senior residents and chiefs. People don’t usually make mistakes because of physical exhaustion. They do so because they’re mentally exhausted.
I read recently that when asked how he would spend an hour, if that was all he had in which to come up with a way to save the world, Einstein said he would spend 55 minutes formulating the problem into a question, and only 5 minutes answering it.
Perhaps if we made that distinction between mental and physical exhaustion in our discussion of work hours vs learning vs patient safety, we might come up with better and more workable solutions for all aspects of the problem.
Cat juggling
July 3, 2009 at 5:35 am | Posted in Uncategorized | 4 CommentsWow, a year away from surgery has done bad things to my stamina. More mentally than physically, but both still need work. Yesterday was only a twelve hour day, and yet by the end I could hardly think straight. I’ll have to build it back up again, and quickly.
It was partly my sleep schedule, which had gotten way off kilter such that I woke up at 1am and couldn’t get back to sleep. But even so, I shouldn’t have been that tired. I think the real problem is that my cat thinks I’m a large toy when I’m asleep, and likes to pounce on my face and torso, claws extended, at random times throughout the night. Which isn’t great for sleep quality.
I may have to kick her out of the room at night. Or have her declawed so that I don’t have to be so hypervigilant about an accidental claw to the eye while I’m sleeping. Declawing is probably the more humane option in this particular situation. But God, from the reaction of the shelter people to the idea of declawing, it’s like you’re threatening to murder small children. I mean, come on! What’s crueler in the end, nightly isolation from her human in addition to all the hours I’m away in the day, or a one-time procedure under anesthesia to amputate the front claws of an entirely indoor cat?
Yes, I said amputate. I know you people use the word as an emotional appeal, to evoke images of a barbaric and painful procedure. But I’m a surgeon; I know exactly what it involves, and it’s no more barbaric than spaying when done correctly under anesthesia. And make no mistake, we spay and neuter primarily for our benefit, to control the number of cats who become feral, and ensure that the population doesn’t exceed our ability to care for them.
Declawing is no different, in that it enables me to give her a better quality of life without jeopardizing my health and safety. In any event, I don’t see a better solution at this time.
(Note: Actual cat juggling is wrong. Also not funny, unlike Steve Martin’s stand up routine about it.)
Facepalm
July 2, 2009 at 4:00 am | Posted in Uncategorized | Leave a commentOrientation is a necessary evil, I guess. But really, how many times do I need a review of OSHA regulations and handwashing? Or HIPAA? Well, I’ll admit I haven’t had quite as many reviews of HIPAA. But my training on its bastard cousin HIPPA has been so frequent that I now despair even about graduate and professional education here in the U.S.
So I entertained myself yesterday with a comparison of how different institutions emphasize different things in their orientations. Where I was before, their main goal was to get everyone ready to work on Day 1. So we got set up with pagers and chart access, scrubs and labcoats, door codes, dictation codes and cheat sheets, and lots of talks about what to expect on the service, professionalism, etc.
Here we did bloodborne pathogen training, basic network access but not chart access, nametags, insurance cards, work/life balance, ACGME competencies, the standard HIPAA {“HIPPA”} presentation, and had a discussion of appropriate prescribing practices. But nothing in terms of getting what we need to do the actual work of a physician. No chart access, no scrubs, no lab coat, no pager.
Fortunately I had some free time in the afternoon while everyone else was off getting oriented at a hospital where I won’t be rotating. So I got all of that done. But had that not been the case, I would have been woefully unprepared to work today.
Hurricane Jill regrets the error
June 30, 2009 at 5:08 pm | Posted in Uncategorized | Leave a commentThe date for the post “Not a moment too soon” has been changed to June 8. Apparently delayed publication on WordPress works differently than it does on Blogger. On the old site, when you saved a post and published it later, the date remained that on which the post was created. Which I like, as it gives a better sense of continuity for the overall narrative of this blog.
Apparently WordPress changes it to the date you decide to publish it. Which I don’t like. Future delayed posts will be dated according to when they were created.
A new treasure trove of funnies
June 30, 2009 at 5:00 pm | Posted in Uncategorized | 3 Comments
Those of you with PhDs, or who have friends with PhDs, will enjoy this site.
Cyberstalking
June 30, 2009 at 5:06 am | Posted in Uncategorized | Leave a commentSo, the agenda for today: lots and lots of reading. On the chairman’s recommendation, I’m skipping all the watered down neurosurgical texts and diving right into that 5000-plus page behemoth known as Youmans Neurological Surgery. And ominously, the first thing that struck me about it was the brevity and precision of the writing. Continue Reading Cyberstalking…
Blog at WordPress.com.
Entries and comments feeds.